The next big Covid-19 variant could begin spreading in New Zealand weeks before we detect it, experts fear, because of "patchy" genomic surveillance amid the Omicron wave.
Whole genomic sequencing – which creates a genetic fingerprint of a given Covid-19 infection – has played a critical part in our pandemic response.
It's helped officials solve mystery incursions, untangle complex chains of transmission and keep a watch on what variants are lurking in our communities.
"Basic science questions like how fast the virus is mutating, where it's mutating, and which mutations matter to spread of the virus have almost exclusively been informed by genetic surveillance," University of Auckland computational biologist Dr David Welch said.
"New Zealand is part of this because we've got mutations that are being expressed here – so we've got to hold up our end of the global effort."
But Welch is now worried our oversight was slipping.
While laboratories were trying to sequence virtually every case in our elimination era, a tsunami of Omicron infections has meant just a fraction of samples from the community were being analysed now.

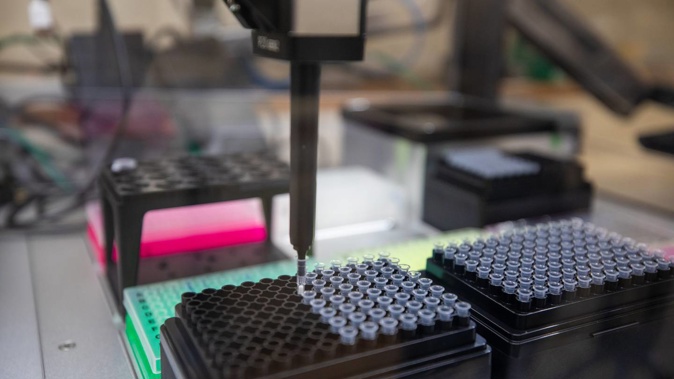
Just a fraction of New Zealand's Covid-19 cases are undergoing whole genome sequencing. Photo / Dom Thomas/RNZ POOL
Of 595,243 positive cases recorded in ESR's EpiSurv system between December 14 and March 28, only 6,341 – or 1.1 per cent – were forwarded to ESR for sequencing.
Over the last two weeks, just 825 or 0.4 per cent of some 232,556 cases, have had at least one sample forwarded – with border cases accounting for around 60 per cent of those.
The Ministry of Health told the Herald that, with new community cases now averaging around 15,000 a day - many of which were being self-reported through rapid antigen testing - it was "no longer possible" to sequence every case.
PCR testing was still being carried out to confirm positive rapid antigen tests for all international arrivals, to help the country keep a watch on variants, as well as "selected" community cases.
Under our current strategy, priority groups for sequencing included all border cases; suspected reinfections; people from previously Covid-free areas; cases possibly acquired in healthcare and among high-risk groups; or unusually severe ones, particularly among the vaccinated.
Secondary to those groups, DHBs were being asked to send samples of randomly-selected positive swabs to ESR – something aimed at providing a representative picture of infection and accounting for factors like location, age, ethnicity and vaccination and sociodemographic status.
Despite those stated checks and measures, Welch saw room for improvement.
"As a gold standard, the World Health Organisation recommends that between 10 and 15 per cent of all cases should be sequenced," he said.
"With current systems, we're only sequencing a very small fraction – or just four or five hundred cases a week."
While just a third of hospitalised cases were being sequenced, Welch said our coverage of such serious infections should be closer to 100 per cent.
"There also appears to be a breakdown with diagnostic labs, which are still picking up more than 400 cases a day with PCR tests – but many of these positive swabs just aren't being sent on for sequencing right now," he said.
"It does take a while for a diagnostic lab to process those samples – but then they also need to physically package them and send them off to ESR, which takes resources.
"If those labs are over-stretched and not actually funded to do that work, and it's largely based on goodwill, they won't do it if they don't have capacity."
Welch said geographic coverage was particularly patchy at present.
"So, there might be a new variant in some DHB area that's putting people in hospital and making them sicker, but we don't know about it yet," he said.
"The other risk is cases coming across the border. We could be looking at a recombination event that occurs overseas and gives the virus an advantage that leads to a new variant.
"Because we're not sequencing 100 per cent of hospitalised cases and recent arrivals from overseas, we just won't know whether they've arrived here or not."
Otago University virologist Dr Jemma Geoghegan echoed those worries.
"We need to know about all hospitalised cases - and we need to know about all border cases."
Asked about the threat at the border, the ministry told the Herald it still had a "high degree of confidence" that any new variants arriving at the border would be identified.
But Welch and Geoghegan remained concerned it could still take time to find a variant once it did get here.
"If there was a new variant known around the world, it could still be ages before we detected it in New Zealand, given the tiny proportion of cases that we're sequencing right now," Geoghegan said.
And when influenza and measles returned to the country, the need would become even more pressing, she said.
Welch added: "With current sequencing coverage, something could be circulating here for many weeks before being detected.
"A large part of our Covid response has been based around having information early and being able to act quickly. Low sequencing coverage jeopardises that."
Ultimately, Welch said there needed to be a "concerted effort" that ensured the country was achieving a higher level of coverage, with all parties in the process committing to a transparent plan.
"So far, it's been a little bit cobbled together, but it's worked fairly well through most of the pandemic," he said.
"I think it was during the height of the Delta outbreak that things started falling apart – and we never got back to that high level of sequencing where we wanted to be."
The ministry said its guidelines for whole genome sequencing of non-border cases were "reviewed and adapted as necessary", both to ensure needless sequencing wasn't carried out, and to ensure demand didn't exceed capacity.
Genomic sequencing wasn't the only area of Covid-19 that experts want to see urgently beefed up.
Last month, modellers said New Zealand was "flying blind" without an ongoing infection prevalence survey like that run by the UK's Office of National Statistics (ONS).
Designed to directly estimate the number of infections in the population, the survey drew on a pool of 150,000 weekly samples to offer regular snapshots of daily infection numbers, along with the percentage of Britons testing positive for Covid-19 antibodies.
The ministry was planning to establish a New Zealand survey over coming months, but it wasn't yet clear whether it would run longitudinally, like the UK's.
- Jamie Morton, NZ Herald
Take your Radio, Podcasts and Music with you








