

Dementia is on the rise in New Zealand, but it is still a condition many are afraid to talk about. In the second of a Northern Advocate series, Denise Piper shines a light on how Alzheimer’s disease and other dementia types impact Northlanders, early warning signs and what help is available in the early stages.
Bruce Willis has plenty of fans in the Tikipunga headquarters of Dementia Tai Tokerau.
Lead community adviser Cindy Faulkes says the Die Hard star’s public battle with dementia has helped to remove the stigma of the progressive brain disorder, especially among men.
The spotlight on the struggles of rugby stars such as Carl Hayman and Bruce Robertson has also helped.
“There’s still a fair amount of stigma out there - people don’t want to get dementia or ‘go doolally’,” she says.
“Notable figures in rugby who have been upfront with it, and Bruce Willis, that has helped open things up, for men in particular.”
Dementia has long been thought to be underdiagnosed in New Zealand, but exact numbers are only being quantified now.
One study under way is the Impact of Dementia mate wareware and Solutions for Equity in Aotearoa, or Idea project for short, which is analysing Pākehā, Chinese and Indian people over 65 in Auckland and Christchurch.
About halfway into the three-year study, interviews with more than 1000 people have identified more than 100 with dementia symptoms, says lead researcher Professor Ngaire Kerse, a director of the University of Auckland’s Centre for Co-Created Ageing Research and the Joyce Cook chair in Ageing Well.
Between a third and half of those identified were not diagnosed with dementia, nor were they receiving the support they needed, she says.

Professor Ngaire Kerse, University of Auckland researcher and the Joyce Cook chair in Ageing Well, says a third to half of people found to have dementia symptoms had not been diagnosed.
Why is dementia underdiagnosed?
Kerse says there could be many reasons for the underdiagnosis, including stigma around dementia.
“Maybe they aren’t aware that there’s an issue. Maybe they’re experienced quite significant stigma, or their families wanted to protect their loved ones from the stigma.”
Another reason could be that people feel they’re managing all right, although Kerse’s team has been busy connecting those identified as having dementia with support services.
Faulkes agrees that many people put off getting a dementia diagnosis, either for themselves or for a loved one, because of fear or stigma.
Another problem is that the progressive condition can be hard for GPs to diagnose, with a need to rule out other things that could be causing memory problems, such as delirium caused by infection.

Bruce Willis was often playing the tough guy in movies like Cosmic Sin, but publicity about his personal battle with frontotemporal dementia is helping other men get a diagnosis.
“And then there’s the problem that you can’t exactly get a living brain and open it up to see what’s happening inside. MRIs can help, with a combination of assessments based on what the person could do and what they can do now.”
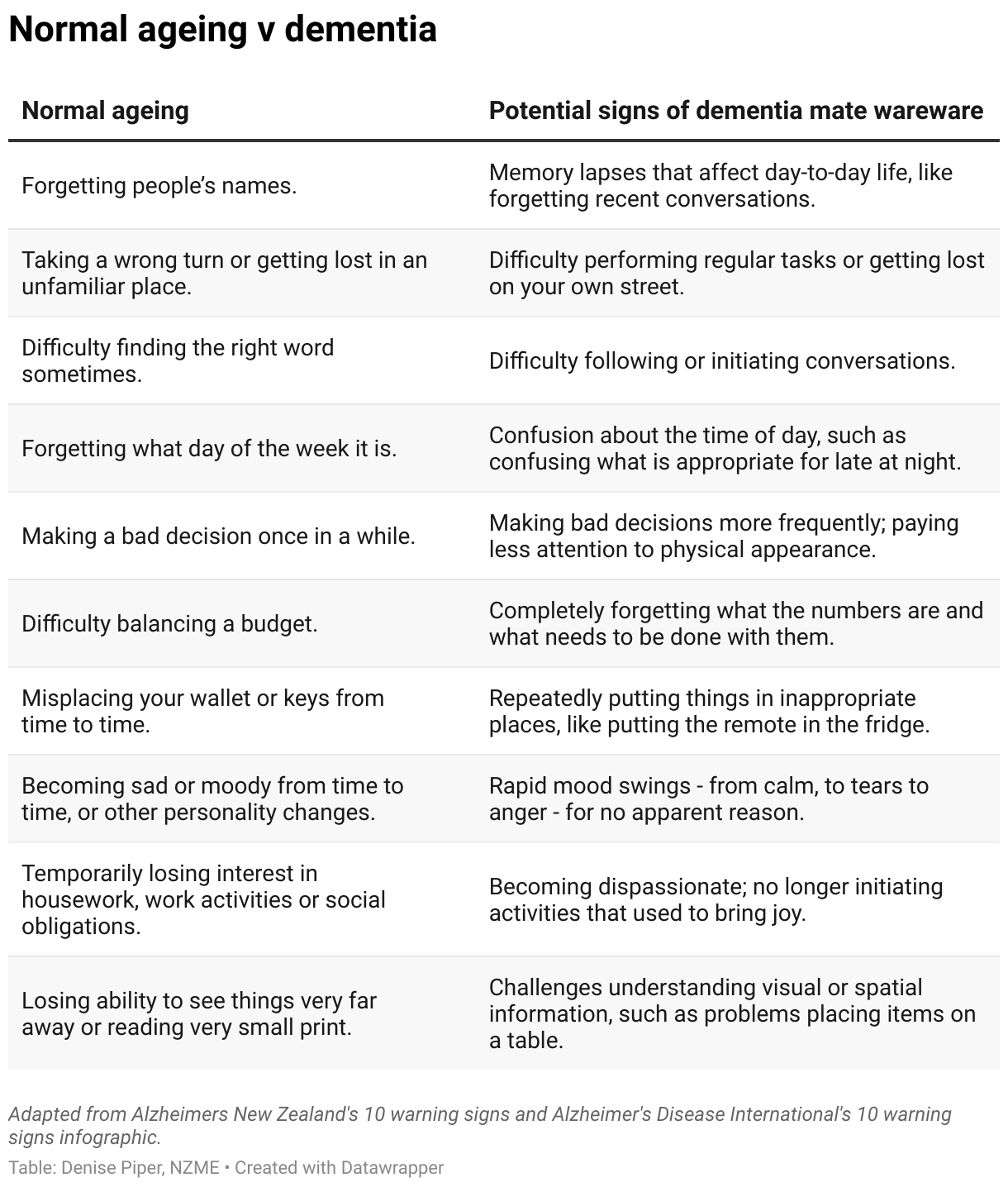
Doctors are looking for not just a bit of memory loss, but significant changes in what a person can remember or can do.
What if a person doesn’t want to see the doctor?
Faulke says another difficulty is when a person knows there is something wrong with their loved one but cannot convince them to see a doctor.
These people are advised to encourage their loved ones to get a warrant of fitness test, or say they need support for their own check-up.

Lead community adviser Cindy Faulkes says Dementia Tai Tokerau, previously called Alzheimers Northland, can help whānau after a diagnosis. Photo / Michael Cunningham Photography
Whatever the case, putting your head in the sand and ignoring the problem only works for so long, Faulke says.
“It makes it really difficult to plan for good health ahead.”
Why it’s best to get an early diagnosis
Despite the fear, it is better to be proactive and know sooner rather than later, says Faulkes, who is not only a community adviser but also helped to look after her father when he had dementia.
An early diagnosis allows the patient to have more say in their care, such as setting up an enduring power of attorney, and their spouses or caregivers can have support.
An age-old fear that people with dementia would be thrown in a care home is not a reality, she says, not least because there are not enough beds for everyone with the condition.
“The reality is we try to keep the person at home for as long as possible. It’s the most economical solution and also what the person wants.”
Help can include medication and day programmes, such as those run by Dementia Tai Tokerau at Alz House in Tikipunga.
There can also be in-home support for daily activities such as taking medication, preparing meals or personal care.
If you are worried that you, or someone you know, is showing signs of dementia mate wareware, see your GP or primary health care provider for a full assessment.
Denise Piper is a news reporter for the Northern Advocate, focusing on health and business. She has more than 20 years in journalism and is passionate about covering stories that make a difference.
Take your Radio, Podcasts and Music with you









