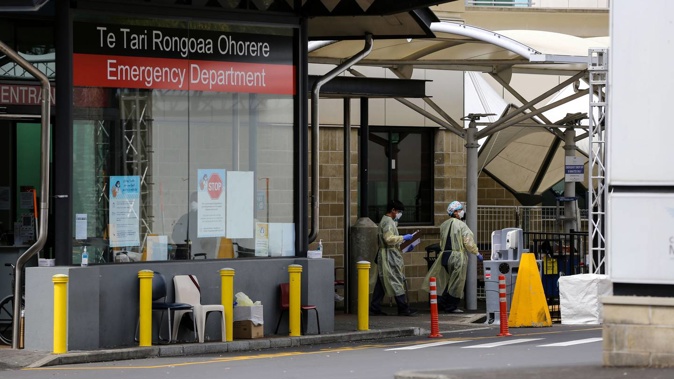
The country's hospitals are facing a perfect storm of Covid-19 and resurgent winter nasties: namely a flu outbreak that's brought the highest patient volumes in a decade. Science reporter Jamie Morton looks at what's causing headaches this winter – and what might be around the corner.
Covid-19
With Covid-19 cases snowballing at a worrying rate across the country, modellers are confident a second Omicron wave is under way.
By Thursday, the seven-day rolling daily case average had jumped to 8013 – from 6114 the week before.
That increase has been similar across the country: on June 22, daily cases per 100,000 were 71.2 in Auckland, 79.3 in Wellington, 97.7 in Canterbury and 103.8 in Southern – but over the next two weeks they leapt to 133.8, 136.3, 178 and 186.4 respectively.
Part of that's down to the relaxing of border restrictions, which has enabled the virus to be liberally seeded across the country at a rate of one new overseas-linked community case each day.
Another big driver is the faster-spreading BA.5 subvariant, which this week may have overtaken BA.2 to become our dominant form of Covid-19 – and may well soon fuel a daily peak of more than 15,000 cases.
ESR's bioinformatics and genomics lead Dr Joep de Ligt anticipated the coming wave to be made up of people contracting Omicron for the first time, but also those suffering their second infections with the variant.
As at this week, 14,000 Kiwis were already known to have contracted the virus twice.
It's known that the vaccine's effectiveness against symptomatic disease can halve over 90 to 180 days – and it's been more than three months since about 2.7 million Kiwis received their booster shot.
"The fact that we're seeing elderly people being affected now is definitely worrisome – but the biggest thing driving hospitalisations internationally is more to do with the actual case count."
De Ligt said it could be that this surge didn't peak until August – with hospitalisations peaking some time after that – but much depended on what measures the Government put in place to slow spread.
Influenza
Because 2020's lockdown effectively wiped out influenza in New Zealand, its return through reopened borders was always going to be a major headache.
In a normal year, the flu infects around one in four Kiwis and kills perhaps 500 – making it hitherto our single deadliest infectious disease before Covid-19 emerged.
ESR surveillance data showed flu began widely spreading around the country in May, before pushing case numbers over June in some places to more than four times what they saw across recent years.
ESR virologist Dr Sue Huang said this year's hospital influenza activity had been the highest observed in a decade.
The bulk of cases have been the familiar influenza A (H3N2 and H3N3), which typically causes more illness in elderly populations – but there's been comparatively little influenza B, which often affects younger and school-aged children.
At Whangarei Hospital, a "twindemic" of Covid-19 and flu has led to patients waiting in tents outdoors and treated in corridors.
/cloudfront-ap-southeast-2.images.arcpublishing.com/nzme/6CTZ3SKMOT7QPFFUJYUS6XZRN4.jpg)
This graph shows patients with severe acute respiratory illnesses (SARI) in hospitals that have tested positive for influenza over recent months, with comparisons to previous years. Source / ESR
While flu remains the most-commonly detected virus through ESR's severe acute respiratory infection (Sari) monitoring – the latest Auckland testing data showed it had been accounting for twice the number of Covid-19 patients – there are signs the surge might have peaked last month.
"It seems to have peaked but it's still too early to say at the moment, because it's only July – and July and August is normally our peak season," Huang said.
Immunisation Advisory Centre director Dr Nikki Turner also noted this season's earlier kick-off.
One factor in rampant flu cases was a lack of uptake: only about 1.1 million Kiwis have received their flu jab - and about a third of Kiwis aged over 55 remain unvaccinated against the virus.
Of course, another was a long stretch without the burden of flu – something that helped boost average life expectancy over the past two years, but has also left us with diminished immune memory.
"We've had no flu for two years, so that's why we're getting quite a nasty one this time," Turner said, adding circulating Covid-19 could have also made flu infections worse this year.
Huang couldn't rule out another wave of flu cases later in the year – especially if influenza B made a comeback.
RSV
Soon after New Zealand opened a travel bubble with Australia last year, the country got slammed a large and severe wave of respiratory syncytial virus, or RSV: a highly contagious disease that causes lung and respiratory tract infections.
More than 6000 cases were reported here, but the true size of the outbreak was likely much bigger because of under-reporting.
Again, the likeliest reason for the surge – which led to children being treated in hospital corridors – was a population that'd grown immunonaive through closed borders and public health measures.
In the latest monitoring week, only about 45 RSV cases were reported to ESR – and Huang said it was likely 2021's outbreak had provided some immunity.
"My guess is this year won't be as bad as last year for RSV," she said.
"But RSV often comes a little later than the flu, so cases could soon start to increase."
/cloudfront-ap-southeast-2.images.arcpublishing.com/nzme/CM7LHZHSZUVPTRA243HAH2T7LI.jpg) ESR virologist De Sue Huang says there are signs the current flu surge may have peaked. Photo / Mark Mitchell
ESR virologist De Sue Huang says there are signs the current flu surge may have peaked. Photo / Mark Mitchell
Dr Vanessa Thornton, director of hospital services for Te Whatu Ora - Counties Manukau, said Middlemore Hospital remained under pressure from a combination of RSV, Covid-19 and flu.
"We expect the impact of these winter illnesses will remain high in our district for another two months."
Norovirus
Although it's sometimes called "winter vomiting bug" overseas, norovirus traditionally doesn't follow seasonal patterns in New Zealand.
That said, ESR has been tracking an unusual spate of norovirus outbreaks around the country over recent weeks. In mid-May, Hawke's Bay Hospital placed a ward in precautionary lockdown to curb spread of the highly contagious bug.
Unlike measles and Covid-19, norovirus isn't a notifiable disease – but it's often detected through outbreaks of acute gastroenteritis, which is one.
ESR senior scientist Dr Joanne Hewitt said 36 outbreaks were reported to the lab in May and 17 in June, with nearly half and almost three quarters of those cases, respectively, occurring in early childcare centres.
Normally, she said, the bulk of norovirus flare-ups happened in aged-care facilities – and the difference for the change this year was unclear.
It also wasn't clear whether the spate would carry on through winter – or beyond.
"It's too early to say what it'll do."
Measles and whooping cough
Otago University virologist Dr Jemma Geoghegan said plenty more nasties were waiting to creep back into our communities.
"It's inevitable that things that've been absent for the past two years are going to be reintroduced."
/cloudfront-ap-southeast-2.images.arcpublishing.com/nzme/5PXIPAQP2WQHTJLQNDX3D4YC7I.jpg) New Zealand hasn't seen any reported cases of measles since early 2020. Image / 123RF
New Zealand hasn't seen any reported cases of measles since early 2020. Image / 123RF
Months after the first national lockdown, scientists tracked big drops in recorded human metapneumovirus (down 92.2 per cent), enterovirus (down 82.2 per cent), adenovirus (down 81.4 per cent) and types one to three of parainfluenza virus (down 80.1 per cent).
The main cause of the common cold, rhinovirus, was also down 74.6 per cent.
While these illnesses had bounced back to resume circulating widely in our communities, measles - a highly contagious disease that caused a serious epidemic in 2019 - hasn't been recorded here since early 2020.
As at March 2022, nearly a third of 18-month-olds – and a similar proportion of children aged 4 and a half years – hadn't completed their immunisations.
Turner said there'd been a drop-off in childrens' coverage rates after 2018, and the pandemic had caused more disruption.
With gaps across children today, and young adults who missed their shots 20 years ago, "we've got quite a high risk that we'll see measles again in New Zealand".
Whooping cough – currently hovering at baseline levels, but known to spike in outbreaks every four to six years – could also make a come-back.
"The thing about whooping cough is little kids get it really badly – so it's important for little kids to get their vaccines on time to protect against severe cases," Turner said.
At Middlemore Hospital, Thornton issued her own appeal to the public.
"Please get vaccinated against the flu, and if you are eligible please get the Covid booster vaccination," she said.
"Stay home if you are unwell and keep up the hygiene standards we've all become familiar with - such as regular hand washing and wearing a mask in public places and on public transport."
Take your Radio, Podcasts and Music with you









